FILE – In this Monday, March 15, 2021 file photo, a health worker applies a dose of the Sinovac vaccine from her vehicle, in the Kalunga Vao de Almas community, a rural area on the outskirts of Cavalcante, Goias state, Brazil. Less than 1% of the world’s poorest citizens have received a dose, and experts say it could be 2023 until vaccines are widely available everywhere. (AP Photo/Eraldo Peres)
PARIS (AP) — No one disputes that the world is unfair. But no one expected a vaccine gap between the global rich and poor that was this bad, this far into the pandemic.
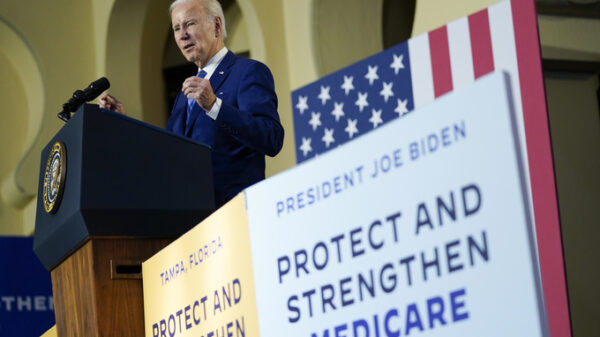
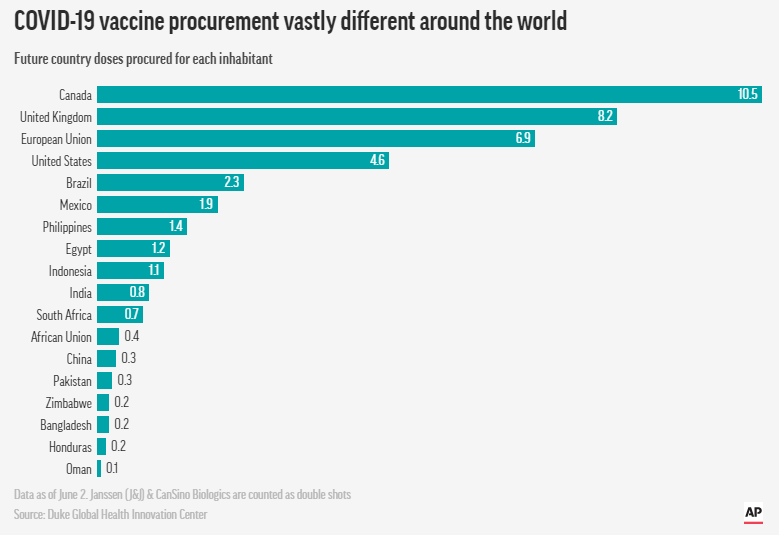
Inequity is everywhere: Inoculations go begging in the United States while Haiti, a short plane ride away, received its first delivery July 15 after months of promises — 500,000 doses for a population over 11 million. Canada has procured more than 10 doses for every resident; Sierra Leone’s vaccination rate just cracked 1% on June 20.
It’s like a famine in which “the richest guys grab the baker,” said Strive Masiyiwa, the African Union’s envoy for vaccine acquisition.
In fact, European and American officials deeply involved in bankrolling and distributing the vaccines against coronavirus have told The Associated Press there was no thought of how to handle the situation globally. Instead, they jostled for their own domestic use.
But there are more specific reasons why vaccines have and have not reached the haves and have-nots.
COVID-19 unexpectedly devastated wealthy countries first — and some of them were among the few places that make the vaccines. Export restrictions kept the doses within their borders.
There was a global purchase plan to provide vaccines for poorer countries, but it was so flawed and underfunded that it couldn’t compete in the cutthroat competition to buy. Intellectual property rights vied with global public health for priority. Rich countries expanded vaccinations to younger and younger people, ignored the repeated pleas of health officials to donate their doses instead and debated booster shots – – even as poor countries couldn’t vaccinate the most susceptible.

The disparity was in some ways inevitable; wealthy nations expected a return on their investment of taxpayer money. But the scale of the inequity, the stockpiling of unused vaccines, the lack of a viable global plan to solve a global problem has shocked health officials, though it wasn’t the first time.
“This was a deliberate global architecture of unfairness,” Masiyiwa told a Milkin Institute conference.
“We have no access to vaccines either as donations or available for us to purchase. Am I surprised? No, because this is where we were with the HIV pandemic. Eight years after therapeutics were available in the West, we did not receive them and we lost 10 million people.”
“It’s simple math,” he said. “We have no access. We have no vaccine miracle.”
The World Health Organization has duly updated its epidemic playbook after every outbreak, most recently with Ebola in mind. Then, as often in the decades before, an emerging illness was largely contained to countries lacking robust public health services, with poor sanitation and crowded living conditions and limited travel connections.
For years, the WHO assessed countries’ readiness for a flu pandemic: The United States, European countries and even India ranked near the top. The U.S. readiness was 96%, and Britain at 93%.
On Jan. 30, 2020, WHO declared the coronavirus outbreak in China to be a global emergency. It would be months before the word “pandemic” became official.
But that same day, the Coalition for Epidemic Preparedness and Innovations, or CEPI, was planning for the worst. CEPI announced “a call for proven vaccine technologies applicable for large scale manufacturing,” according to minutes from its scientific advisory group. CEPI said it would be critical “to support the strategy for global access” early in the game.
CEPI quickly invested in two promising coronavirus vaccines being developed by Moderna and CureVac.
“We said very early on that it would be important to have a platform where all countries could draw vaccines from, where there’s accountability and transparency,” said Christian Happi, a professor at Nigeria’s Redeemer’s University and a member of CEPI’s scientific advisory committee. “But the whole idea was that we thought rich countries would fund it for the developing world.”
Happi said officials never expected the pandemic would strike first and hardest in Europe and the U.S. Or that their assessment of preparedness in the world’s most advanced economies would prove horrifically optimistic.
Global health experts would soon come to realize that rich countries “could sign a piece of paper saying they believe in equity, but as soon as the chips are down, they will do whatever they want,” he said.
On March 16, five days after the global pandemic was declared, the novel mRNA vaccine developed by Moderna was injected into a trial participant for the first time.
By then, the disease was tearing through the elderly populations of Europe and the United States.

Moderna and Pfizer/BioNTech were the first companies to come out with an mRNA vaccine, devising methods of mass production almost on the fly. Scientists at Britain’s Oxford University also came up with a vaccine with a more traditional platform, and Bill Gates brokered a deal for them to partner with AstraZeneca, a pharmaceutical company with global reach but no experience in vaccine production.
On April 30, the deal was confirmed: AstraZeneca took sole responsibility for the global production and distribution of the Oxford vaccine and pledged to sell it for “a few dollars a dose.” Over the next few weeks, the U.S. and Britain secured agreements totaling 400 million doses from AstraZeneca.
The race to make and secure vaccines was on, and the United States and Britain were leagues in front of the rest of the world — a lead they wouldn’t lose. Still, both countries would see life expectancy decline by at least a year in 2020, the biggest drop since World War II. In the European Union, 22 countries saw their average lifespans cut short, with Italy leading the list.
But as grim as the situation was, all those countries had a major advantage: They were home to the pharmaceutical companies with the most promising vaccine candidates, the world’s most advanced production facilities, and the money to fund both.
On May 15, 2020, President Donald Trump announced Operation Warp Speed and promised to deliver vaccines against coronavirus by New Year’s. With unparalleled money and ambition behind the project, Warp Speed head Moncef Slaoui was more confident than his counterparts in Europe that a vaccine was in the offing. He signed contracts almost without regard to price or conditions.
“We were frankly focused on getting this as fast as humanly possible. If I had to redo it, I probably should have voiced more of a global dimension,” said Slaoui. “The operation had focused, which was frankly also part of its success, on staying out of the politics and making the vaccines.”
The idea of including clauses to ensure that vaccines would go to anyone besides Americans wasn’t even considered.
At the same time, the U.S. repeatedly invoked the Defense Production Act — 18 times under the Trump Administration and at least once under Biden. The moves barred exports of crucial raw materials as factories were ramping up production of the as-yet-unapproved vaccines — and eventually, of the vaccines themselves.
But it also meant those materials would run low in much of the rest of the world. The U.S. stranglehold would lift only in spring 2021, and only partially.
Operation Warp Speed supercharged the global race to secure vaccines, but it would still take another two weeks until COVAX — the COVID-19 Vaccines Global Access Facility — was formally announced as the entity to ensure equity, with the Serum Institute of India as the core supplier for the developing world.
COVAX had the backing of the World Health Organization, CEPI, vaccines alliance Gavi and the powerful Gates Foundation. What it did not have was cash, and without cash it could secure no contracts.
“Operation Warp Speed signed the first public deals and that started a chain reaction,” said Gian Gandhi, UNICEF’s COVAX coordinator for supply. “It was a like a rush on the banks, but to buy up the expected supply.”
Some involved in the COVAX project flagged India as a potential problem early on, according to minutes of meetings in late spring and early summer of 2020.
India’s government had blocked exports of protective gear, but many global health authorities who hadn’t fully grasped the extent of pandemic nationalism found it unimaginable that the country would block vaccines when the world was counting on them. Also, India had so far been spared the waves of death that were sweeping across Europe and the Americas.

A separate plan put forward by the government of Costa Rica and the World Health Organization to create a technology-sharing platform to expand vaccine production foundered. Not a single company agreed to share its blueprints, even for a fee — and no government pushed them behind the scenes, according to multiple people involved in the project.
On the global scale, the one organization that could have pushed for more technology sharing was the Gates Foundation, whose money to WHO nearly matches that of the U.S. government.
Instead, Bill Gates defended stringent intellectual property rights as the best way to speed innovation. His foundation poured money and influence into the Access to COVID-19 Tools Accelerator, which also failed to generate the money or influence needed to ramp up production outside already existing hubs.
In the United States, meanwhile, manufacturing and the trials went on in parallel, which is where taxpayers and the companies took enormous risks that paid off for both.
But in retrospect, Slaoui said, given the sheer amount of taxpayer money involved, each time they signed new contracts the U.S. and other countries could have pushed companies harder to share their knowledge, if only for the duration of the pandemic.
“From a geopolitical standpoint, it’s critical that they do that,” he said.
Nowhere was the situation more dire than Africa. In February, WHO’s African expert in vaccine development, Richard Mihigo, was among many who said the continent’s experience with other pandemics had uniquely prepared it for a complex vaccine deployment.

Five months later, contemplating the plight of a continent that gets 99% of its vaccines from abroad, Mihigo adds a rueful footnote: “One of the lessons we learned from this pandemic is how badly prepared we were in vaccine production in the region and how dependent we were on imports.”
Those imports have only barely begun to materialize — and they are insufficient to meet even the limited goals of the COVAX initiative to vaccinate at least 20% of the population of 92 low- and middle-income countries by the end of this year.
From the start, the coalition of organizations that created COVAX found themselves fighting the last war.
The plan was designed as an international pool to spur demand for vaccines and treatment of diseases with a relatively small global footprint, said Winnie Byanyima, head of UNAIDS.
Something like Ebola. But the coronavirus pandemic looked nothing like an Ebola outbreak.
“That itself was a structural weakness,” she said.
Although the World Bank and the International Monetary Fund had between them set aside billions for vaccinating the developing world, that money was intended to go to countries and was out of bounds for a global vaccine sharing plan like COVAX, said Mike Muldoon, managing director for innovative finance at the Rockefeller Foundation.
Meanwhile, governments competed to secure contracts for vaccines by the hundreds of millions.
On Dec. 8, Britain became the first country to formally authorize a start to widespread vaccinations, injecting 90-year-old Margaret Keenan with a dose of the Pfizer-BioNTech vaccine. Six days later, the United States started its own vaccinations. And on Dec. 26, the EU followed suit. China and Russia had been vaccinating even before releasing data from their homegrown inoculations.
Maria Cheng reported from London, and Aniruddha Ghosal from New Delhi. Other contributors include Sally Ho in Seattle; Zeke Miller in Washington; Danica Coto in San Juan, Puerto Rico; and Stacey Plaisance in New Orleans.
Copyright 2020 Associated Press. All rights reserved.
Source: https://apnews.com/article/coronavirus-vaccine-inequality-dac9c07b324e29d3597037b8dc1d908a