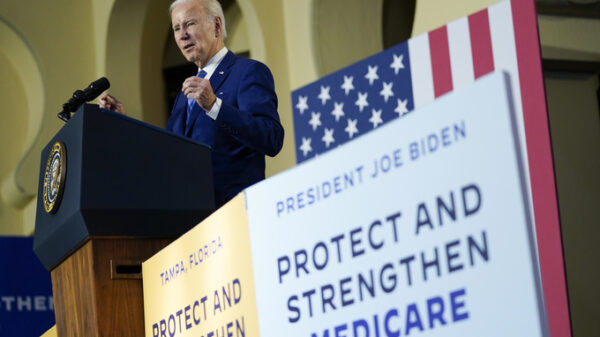
A COVID-19 patient receives treatment in the ICU of the Hospital del Mar, in Barcelona, Spain, Tuesday, Jan. 19, 2021. The unrelenting increase in COVID-19 infections in Spain following the holiday season is again straining hospitals, threatening the mental health of doctors and nurses who have been at the forefront of the pandemic for nearly a year. (AP Photo/Felipe Dana)
BARCELONA, Spain (AP) — The unrelenting increase in COVID-19 infections in Spain following the holiday season is again straining hospitals, threatening the mental health of doctors and nurses who have been at the forefront of the pandemic for nearly a year.
In Barcelona’s Hospital del Mar, the critical care capacity has more than doubled and is nearly full, with 80% of ICU beds occupied by coronavirus patients.
“There are young people of 20-something-years-old and older people of 80-years-old, all the age groups,” said Dr. Joan Ramon Masclans, who heads the ICU. “This is very difficult, and it is one patient after another.”
Even though authorities allowed gatherings of up to 10 people for Christmas and New Year celebrations, Masclans chose not to join his family and spent the holidays at home with his partner.
“We did it to preserve our health and the health of others. And when you see that this isn’t being done (by others) it causes significant anger, added to the fatigue,” he said.
A study released this month by Hospital del Mar looking at the impact of the spring’s COVID-19 surge on more than 9,000 health workers across Spain found that at least 28% suffered major depression. That is six times higher than the rate in the general population before the pandemic, said Dr. Jordi Alonso, one of the chief researchers.
In addition, the study found that nearly half of participants had a high risk of anxiety, post-traumatic stress disorder, panic attacks or substance- and alcohol-abuse problems.
Spanish health care workers are far from the only ones to have suffered psychologically from the pandemic. In China, the levels of mental disorders among doctors and nurses were even higher, with 50% reporting depression, 45% reporting anxiety and 34% reporting insomnia, according to the World Health Organization.
In the U.K., a survey released last week by the Royal College of Physicians found that 64% of doctors reported feeling tired or exhausted. One in four sought out mental health support.
“It is pretty awful at the moment in the world of medicine,” Dr. Andrew Goddard, president of the Royal College of Physicians, said in a statement accompanying the study. “Hospital admissions are at the highest-ever level, staff are exhausted, and although there is light at the end of the tunnel, that light seems a long way away.”
Dr. Aleix Carmona, a third-year anesthesiology resident in Spain’s northeastern region of Catalonia, didn’t have much ICU experience before the pandemic hit. But as surgeries were cancelled, Carmona was summoned to the ICU at the Moisès Broggi hospital outside Barcelona to fight a virus the world knew very little about.
“In the beginning, we had a lot of adrenaline. We were very frightened but we had a lot of energy,” Carmona recalled. He plowed through the first weeks of the pandemic without having much time to process the unprecedented battle that was unfolding.
It wasn’t until after the second month that he began feeling the toll of seeing first-hand how people were slowly dying as they ran out of breath. He pondered what to tell patients before intubating them. His initial reaction had always been to reassure them, tell them it would be alright. But in some cases he knew that wasn’t true.
“I started having difficulty sleeping and a feeling of anxiety before each shift,” Carmona said, adding that he would return home after 12 hours feeling like he had been beaten up.
For a while he could only sleep with the help of medication. Some colleagues started taking anti-depressants and anti-anxiety drugs. What really helped Carmona, though, was a support group at his hospital, where his co-workers unloaded the experiences they had bottled up inside.
But not everyone joined the group. For many, asking for help would make them seem unfit for the job.
“In our profession, we can handle a lot,” said David Oliver, a spokesman for the Catalonia chapter of the SATSE union of nurses. “We don’t want to take time off because we know we will add to the workload of our colleagues.”
The most affected group of health care workers, according to the study, were nurse’s aides and nurses, who are overwhelmingly women and often immigrants. They spent more time with dying COVID-19 patients, faced poor working conditions and salaries and feared infecting family members.
Desirée Ruiz is the nurse supervisor at Hospital del Mar’s critical care unit. Some nurses on her team have asked to take time off work, unable to cope with the constant stress and all the deaths.
To prevent infections, patients are rarely allowed family visits, adding to their dependency on nurses. Delivering a patient’s last wishes or words to relatives on the phone is especially challenging, Ruiz said.
“This is very hard for … people who are holding the hand of these patients, even though they know they will end up dying,” she said.
Ruiz, who organizes the nurses’ shifts and makes sure the ICU is always staffed adequately, is finding it harder and harder to do so.
Unlike in the summer, when the number of cases fell and health workers were encouraged to take holidays, doctors and nurses have been working incessantly since the fall, when virus cases picked up again.
The latest resurgence has nearly doubled the number of daily cases seen in November, and Spain now has the third-highest COVID-19 infection rate in Europe and the fourth-highest death toll, with more than 55,400 confirmed fatalities.
But unlike many European countries, including neighboring Portugal, the Spanish health minister has for now ruled out the possibility of a new lockdown, relying instead on less drastic restrictions that aren’t as damaging to the economy but take longer to decrease the rate of infections.
Alonso fears the latest surge of virus patients could be as detrimental to the mental health of medical staff as the shock of the pandemic’s first months.
“If we want to be cared for adequately, we also need to take care of the health care workers, who have suffered and are still suffering,” he said.
Copyright 2020 Associated Press. All rights reserved.